OBJECTIVES: The aim of the following study was to assess contour changes after socket preservation techniques.
MATERIAL AND METHODS: In five beagle dogs, the distal root of the third and fourth mandibular premolars was extracted. The following treatments (Tx) were randomly assigned for the extraction socket. Tx 1: BioOss Collagen. Tx 2: BioOss Collagen and a free soft tissue graft. Tx 3: No treatment. Tx 4: The internal buccal aspect was covered with an experimental collagen membrane, the extraction socket was filled with BioOss Collagen and the membrane folded on top of the graft. Impressions were obtained at baseline, 2 and 4 months after surgery. Bucco-lingual measurements were performed using digital imaging analysis.
RESULTS: All groups displayed contour shrinkage at the buccal aspect. Only the differences between the two test groups (Tx 1, Tx 2) and the control group (Tx 3) were significant at the buccal aspect (p< or =0.001). No measurements of the Tx 4 group could be performed.
CONCLUSION: Socket preservation techniques, used in the present experiment, were not able to entirely compensate for the alterations after tooth extraction. Yet, incorporation of BioOss Collagen seems to have the potential to limit but not avoid the post-operative contour shrinkage.
J Clin Periodontol. 2008 Oct;35(10):906-13. Epub 2008 Aug 17.
Ridge preservation techniques for implant therapy (Review JOMI)
PURPOSE:
The aim of this review was to evaluate the techniques and outcomes of postextraction ridge preservation and the efficacy of these procedures in relation to subsequent implant placement.MATERIALS AND METHODS:
A MEDLINE/PubMed search was conducted and the bibliographies of reviews from 1999 to March 2008 were assessed for appropriate studies. Randomized clinical trials, controlled clinical trials, and prospective/retrospective studies with a minimum of five patients were included.RESULTS:
A total of 135 abstracts were identified, from which 53 full-text articles were further examined, leading to 37 human studies that fulfilled the search criteria. Many different techniques, methodologies, durations, and materials were presented in the publications reviewed, making direct comparison difficult.CONCLUSIONS:
Despite the heterogeneity of the studies, it was concluded that ridge preservation procedures are effective in limiting horizontal and vertical ridge alterations in postextraction sites. There is no evidence to support the superiority of one technique over another. There is also no conclusive evidence that ridge preservation procedures improve the ability to place implants.Int J Oral Maxillofac Implants. 2009;24 Suppl:260-71.
Ridge preservation techniques for implant therapy.
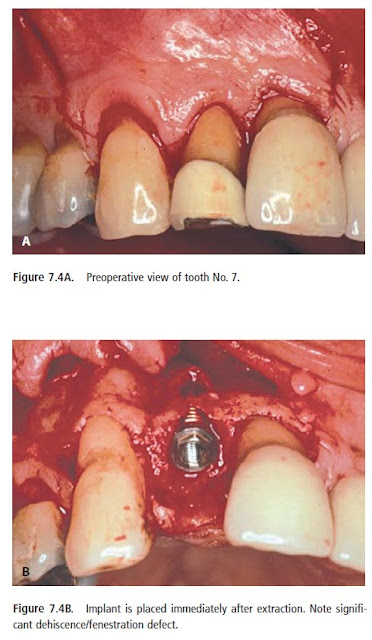
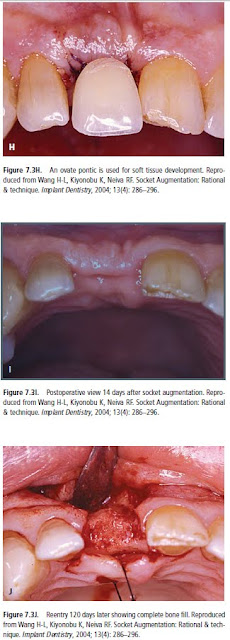
Socket Augmentation: Rationale and Technique (Part 3)
Guided Bone Regeneration (GBR)
Cases in which the buccal plate is absent or was lostduring exodontia require a different approach.GBR techniques associated with or without immediate implant placement are required to treat these ridge
defects. A delayed implant placement approach is indicated when primary stability of the implant cannot be predictably achieved, particularly in sockets of bi- or multirooted teeth.
In these cases GBR techniques, such as the “sandwich bone augmentation,” are indicated (Wang et al. 2004b).
Abd El Salam El Askary, Fundamentals of Esthetic Implant Dentistry, 2007
Socket Augmentation: Rationale and Technique (Part 2)
Layers Technique (when buccal plate is ≤1 mm thickness)
The layers technique was developed to maximize bone healing in sockets with compromised healing potential.
A combination of a bone replacementgraft and a collagen wound dressing material should be used when the buccal socket wall is ≤1 mm thick at approximately 2–3mm below the alveolar crest and/or occurrence of dehiscence or fenestrations are found. Mineralized bone grafts that are quickly replaced by host bone are
preferable.
The bone graft should be tamped down lightly, and overfill should be avoided. Adequate space between the graft particles is critical to allow for revascularization to spread throughout the graft, bringing the proteins and growth factors necessary for new bone growth (Becker et al. 1992, Mellonig 1996).
The histologic data obtained from our unpublished data indicated 68% of vital bone, 5% of residual particle, and 27% of connective tissue. This is similar to the human host bone component. Sites that may also benefit from using this technique include those with thin bone ≤1 mm, periapical pathologies, and sockets of multirooted teeth associated with loss of the interradicular bone.
The histologic data obtained from our unpublished data indicated 68% of vital bone, 5% of residual particle, and 27% of connective tissue. This is similar to the human host bone component. Sites that may also benefit from using this technique include those with thin bone ≤1 mm, periapical pathologies, and sockets of multirooted teeth associated with loss of the interradicular bone.
A combination of a bone replacementgraft and a collagen wound dressing material should be used when the buccal socket wall is ≤1 mm thick at approximately 2–3mm below the alveolar crest and/or occurrence of dehiscence or fenestrations are found. Mineralized bone grafts that are quickly replaced by host bone are
preferable.
The bone graft should be tamped down lightly, and overfill should be avoided. Adequate space between the graft particles is critical to allow for revascularization to spread throughout the graft, bringing the proteins and growth factors necessary for new bone growth (Becker et al. 1992, Mellonig 1996).
The histologic data obtained from our unpublished data indicated 68% of vital bone, 5% of residual particle, and 27% of connective tissue. This is similar to the human host bone component. Sites that may also benefit from using this technique include those with thin bone ≤1 mm, periapical pathologies, and sockets of multirooted teeth associated with loss of the interradicular bone.
The histologic data obtained from our unpublished data indicated 68% of vital bone, 5% of residual particle, and 27% of connective tissue. This is similar to the human host bone component. Sites that may also benefit from using this technique include those with thin bone ≤1 mm, periapical pathologies, and sockets of multirooted teeth associated with loss of the interradicular bone.
Abd El Salam El Askary, Fundamentals of Esthetic Implant Dentistry, 2007
Future posts will describe cases, in which the buccal plate is absent or was lost during exodontia require a different approach
Socket Augmentation: Rationale and Technique
Tooth extraction, either traumatic or atraumatic, results in alveolar bone loss, both in width and height (Bays
1986, Mecall and Rosenfeld 1996, Mecall and Rosenfeld 1992, Mecall and Rosenfeld 1991). An average of 40% to 60% of original height and width is expected to be lost after tooth extraction, with the greatest loss happening within the first year (Sevor and Meffert 1992, Polizzi et al. 2000, Grunder et al. 1999, Werbitt and Goldberg 1992, Werbitt and Goldberg 1991). This can negatively influence bone volume that is needed for future dental implant placement as well as proper ideal esthetic restoration. Research has demonstrated that the alveolar ridge at the maxillary anterior area can be reduced by 23% in the first six months after tooth extraction, and an additional 11% in the following five years (Artzi et al. 2000). In the posterior mandible, resorption happens primarily in the buccal/labial direction, resulting in a lingual displacement of alveolar crest (Artzi et al. 2000).
Traditional Socket Management with or without Collagen Wound Dressing Material (socket management when
buccal plate is ≥1 mm thickness):
1986, Mecall and Rosenfeld 1996, Mecall and Rosenfeld 1992, Mecall and Rosenfeld 1991). An average of 40% to 60% of original height and width is expected to be lost after tooth extraction, with the greatest loss happening within the first year (Sevor and Meffert 1992, Polizzi et al. 2000, Grunder et al. 1999, Werbitt and Goldberg 1992, Werbitt and Goldberg 1991). This can negatively influence bone volume that is needed for future dental implant placement as well as proper ideal esthetic restoration. Research has demonstrated that the alveolar ridge at the maxillary anterior area can be reduced by 23% in the first six months after tooth extraction, and an additional 11% in the following five years (Artzi et al. 2000). In the posterior mandible, resorption happens primarily in the buccal/labial direction, resulting in a lingual displacement of alveolar crest (Artzi et al. 2000).
Traditional Socket Management with or without Collagen Wound Dressing Material (socket management when
buccal plate is ≥1 mm thickness):
Abd El Salam El Askary, Fundamentals of Esthetic Implant Dentistry, 2007
Future posts will describe cases, when buccal plate is ≤1 mm thickness and Cases in which the buccal plate is absent or was lost during exodontia require a different approach
Socket Preservation technique before implant placement
Human mineralized bone in extraction sites before implant placement
After tooth extraction, labial or facial bone loss may be significant, resulting in less-thanideal
bone being available for implant placement. Horizontal or vertical deficiency with
loss of interseptal, mesial or distal bone also may occur, depending on the etiology
leading to tooth extraction, such as severe periodontal disease or chronic
bone loss from tooth fracture. Even after a “clean” extraction, bone loss may be
unpredictable, resulting in limitation of ideal implant placement.
bone being available for implant placement. Horizontal or vertical deficiency with
loss of interseptal, mesial or distal bone also may occur, depending on the etiology
leading to tooth extraction, such as severe periodontal disease or chronic
bone loss from tooth fracture. Even after a “clean” extraction, bone loss may be
unpredictable, resulting in limitation of ideal implant placement.
Major changes of an extraction site take place during the 12 months following tooth extraction. The width of the alveolar ridge was reduced by 50% during the observation period (12 months). This loss, corresponding to 5 to 7 mm, is in agreement with earlier studies. The finding that approximately two thirds of this reduction occurred within the first 3 months after tooth extraction also corresponds to earlier findings.(Lars Schropp, 2003)
In an effort to preserve and create sufficient bone for implant placement after mandibular molar extraction, we have used human mineralized cancellous bone (Puros, Sulzer Dental, Carlsbad, Calif.) as a graft material. For mandibular molar sites, we have used advancement flaps to achieve primary closure, without the use of membranes or collagen. This technique has allowed
for successful placement of implants in molar sites that otherwise may not have had satisfactory amounts of bone for ideal implant placement.
for successful placement of implants in molar sites that otherwise may not have had satisfactory amounts of bone for ideal implant placement.
Background. Bone loss after tooth extraction may prevent dental implant placement. Human mineralized bone grafts can be used to restore bone volume and allow for tooth replacement with dental implants.
Methods. The authors grafted 22 sites in 18 patients with human mineralized bone after tooth extraction. They allowed molar sites 16 weeks for graft healing, placed the implants
and restored them with a final crown after a four-month integration period. Singlerooted
maxillary sites received implants and immediate placement of provisional crowns or underwent a delayed two-stage restoration approach. The authors used radiographs and clinical examinations to evaluate the results.
Results. All of the sites were restored successfully with a single-tooth implant restoration.
Periapical radiographs indicated that the crestal bone levels were limited to
the first thread of the implants or slightly coronal to the first thread of the implant.
Clinical evaluation indicated excellent gingival health around the provisional and
final restorations, without obvious gingival migration.
Conclusions. The use of human mineralized bone may have significant potential to
reconstruct missing bone resulting from tooth extraction and to preserve bone after
tooth extraction. In addition, healed bone graft sites seem to be able to support immediate
placement of a provisional crown and implant restorations.
Clinical Implications. Patients who are having teeth extracted may become candidates
for implant restorations when the sites are appropriately grafted to preserve and reconstruct bone volume, thus allowing for more options for reconstructing the
missing tooth site.
Methods. The authors grafted 22 sites in 18 patients with human mineralized bone after tooth extraction. They allowed molar sites 16 weeks for graft healing, placed the implants
and restored them with a final crown after a four-month integration period. Singlerooted
maxillary sites received implants and immediate placement of provisional crowns or underwent a delayed two-stage restoration approach. The authors used radiographs and clinical examinations to evaluate the results.
Results. All of the sites were restored successfully with a single-tooth implant restoration.
Periapical radiographs indicated that the crestal bone levels were limited to
the first thread of the implants or slightly coronal to the first thread of the implant.
Clinical evaluation indicated excellent gingival health around the provisional and
final restorations, without obvious gingival migration.
Conclusions. The use of human mineralized bone may have significant potential to
reconstruct missing bone resulting from tooth extraction and to preserve bone after
tooth extraction. In addition, healed bone graft sites seem to be able to support immediate
placement of a provisional crown and implant restorations.
Clinical Implications. Patients who are having teeth extracted may become candidates
for implant restorations when the sites are appropriately grafted to preserve and reconstruct bone volume, thus allowing for more options for reconstructing the
missing tooth site.
CASE PRESENTATION
MICHAEL S. BLOCK, D.M.D.; ISRAEL FINGER, D.D.S.,
ROBERT LYTLE, D.D.S.
ROBERT LYTLE, D.D.S.
J Am Dent Assoc 2002;133;1631-1638
Subpontic osseous hyperplasia
The newest publication of subpontic osseous hyperplasia:
Three cases of subpontic osseous hyperplasia of the mandible: a report.
Islam MN, Cohen DM, Waite MT, Bhattacharyya I.
Quintessence Int. 2010 Apr;41(4):299-302.
Subpontic osseous hyperplasia is a relatively uncommon benign submucosal mass of normal bone found beneath a pontic. Three cases of mandibular subpontic osseous hyperplasia are described, adding to the 40 existing cases in the English-language literature. Subpontic osseous hyperplasia may represent a unique reactive osseous metaplasia in the subpontic region, with chronic stimuli and functional or occlusal stress as possible etiologies. This article aims to address the clinical significance, treatment considerations, and radiographic correlation of subpontic osseous hyperplasia.
Radiographic picture:
Three cases of subpontic osseous hyperplasia of the mandible: a report.
Islam MN, Cohen DM, Waite MT, Bhattacharyya I.
Quintessence Int. 2010 Apr;41(4):299-302.
Subpontic osseous hyperplasia is a relatively uncommon benign submucosal mass of normal bone found beneath a pontic. Three cases of mandibular subpontic osseous hyperplasia are described, adding to the 40 existing cases in the English-language literature. Subpontic osseous hyperplasia may represent a unique reactive osseous metaplasia in the subpontic region, with chronic stimuli and functional or occlusal stress as possible etiologies. This article aims to address the clinical significance, treatment considerations, and radiographic correlation of subpontic osseous hyperplasia.
Radiographic picture:
The etiology and prevalence of gingival recession
Background. Gingival recession in its localized or generalized form is an undesirable
condition resulting in root exposure.The result often is not esthetic and may lead to sensitivity and root caries. Exposed root surfaces also are prone to abrasion. The purpose of this article is to describe the prevalence, etiology and factors associated with gingival recession.
Types of Studies Reviewed. The authors reviewed cross-sectional epidemiologic studies of gingival recession and found that they correlated the prevalence of recession to trauma, sex, malpositioned teeth,
inflammation and tobacco consumption. The recent surveys they reviewed revealed that 88 percent of people 65 years of age and older and 50 percent of people 18 to 64 years of age have one or more sites with
recession. The presence and extent of gingival recession also increased with age.
Results. More than 50 percent of the population has one or more sites with gingival
recession of 1 mm or more. The prevalence of gingival recession was found in patients with both good and poor oral hygiene. It has been proposed that recession is multifactorial, with one type being associated with
anatomical factors and another type with physiological or pathological factors. Recession has been found more frequently on buccal surfaces than on other aspects of the teeth.
Clinical Implications. Dentists should be knowledgeable about the etiology, prevalence and associating factors of gingival recession, as well as treatment options, so that appropriate treatment modalities can be offered to patients. Treatments for gingival recession include gingival grafting, guided tissue regeneration and orthodontic therapy. Such treatments typically result in esthetic improvement, elimination of sensitivity and a decreased risk of developing root caries.
Gingival recession is characterized by the displacement of the gingival margin apically from the cementoenamel junction, or CEJ, or from the former location of the CEJ in which restorations have distorted the location or appearance of the CEJ. Gingival recession can be localized or generalized and be associated with one or more surfaces.(Smith RG. 1997) The resulting root exposure is not esthetically
pleasing and may lead to sensitivity and root caries. As a result, we reviewed studies that described the prevalence, etiology and factors associated with gingival recession.
AGING
Similarly, Gorman found that the frequency of gingival recessio increased with age and was greater
in men than in women of the same age. Malpositioned teeth and toothbrush trauma were found to be the
most frequent etiologic factors associated with gingival recession.
Recession associated with labially positioned teeth occurred in 40 percent of patients 16 to 25 years of age
and increased to 80 percent of patients in the 36 to 86 years of age group. Those findings were corroborated
by Murray, who examined 4,000 subjects and found that the incidence of gingival recession increased with age.
ANATOMICAL FACTORS
One etiologic factor that may be associated with gingival recession is a prior lack of alveolar bone
at the site. The deficiencies in alveolar bone may be developmental (anatomical) or acquired (physiological
or pathological).Anatomical factors that have been related to recession include fenestration and dehiscence of
the alveolar bone, abnormal tooth position in the arch, aberrant path of eruption of the tooth and
individual tooth shape. All those anatomical factors are interrelated and may result in an alveolar
osseous plate that is thinner than normal and that may be more susceptible to resorption.
PHYSIOLOGICAL FACTORS
Physiological factors may include the orthodontic movement of teeth
to positions outside the labial or lingual alveolar plate, leading to dehiscence formation.Such
studies suggested that the acquired loss of alveolar bone might be associated with a number of identifiable
physiological or pathological conditions for which bone loss is part of a physiological or pathological
process.
PATHOLOGICAL FACTORS
Pathological factors include bone resorption as a sequel to microbially induced periodontal diseases.
In this case, however, the process of recession may be more complex since the teeth
involved may extrude, tilt and become mobile. A rat study demonstrated a possible mechanism of
gingival recession, showing that loss of attachment was the result of localized inflammatory
processes in connective tissue with the accumulation of mononuclear cells.(Baker DL 1976) It also was suggested that inflammation may persist subclinically and therefore cannot be eliminated as a factor in
recession.Similarly, recession has been related to inflammation in periodontal connective tissue
in monkeys.(Hopps 1974)
TRAUMA
In addition to psychological factors, various forms of trauma—such as vigorous toothbrushing, aberrant
frenal attachment, occlusal injury, operative procedures and tobacco chewing—have been thought to play a role in the etiology of recession.
Traumatic mechanical toothbrushing is factor in the etiology of gingival recession. The effects of toothbrushing have been studied by many investigators with general agreement that vigorous or incorrect use of the toothbrush can produce recession.
HYGIENE
The frequency of gingival recession in subjects with excellent oral hygiene has been reported to
be more frequent at buccal than proximal or lingual surfaces. In an epidemiologic study, gingival
recession was positively correlated with the frequency of toothbrushing.
Recession occurs more frequently in patients with good rather than poor oral hygiene.(O’Leary TJ 1971)
ABERRANT FRENAL ATTACHMENT
Aberrant frenal attachment also has been mentioned as a cause of localized
recession, but the evidence is not overwhelming. Some studies did not find any correlation
between frenal pull and recession, whereas thers did find an association.
The Miller classification system.
A. Class I recession. B. Class II recession. C. Class III recession. D. Class IV recession.
TREATMENT OPTIONS
Different gingival grafting techniques have been proposed to treat gingival recession, including the lateral sliding flaps, coronally positioned flaps and connective tissue grafts, resulting in mean
root coverage of 65 to 98 percent. Guided tissue regeneration was introduced later to treat
recession, using bioabsorbable or nonabsorbable membranes, and studies showed similar results
with a mean root coverage of 48 to 92 percent. Orthodontic treatment can be considered with or
without periodontal surgery, especially in situations were teeth are malpositioned.
The etiology and prevalence of gingival recession
MOAWIA M. KASSAB, D.D.S., M.S.; ROBERT E.COHEN, D.D.S., Ph.D.
J Am Dent Assoc 2003;134;220-225
About different treatment techniques of gingival recession we will talk at future posts.
condition resulting in root exposure.The result often is not esthetic and may lead to sensitivity and root caries. Exposed root surfaces also are prone to abrasion. The purpose of this article is to describe the prevalence, etiology and factors associated with gingival recession.
Types of Studies Reviewed. The authors reviewed cross-sectional epidemiologic studies of gingival recession and found that they correlated the prevalence of recession to trauma, sex, malpositioned teeth,
inflammation and tobacco consumption. The recent surveys they reviewed revealed that 88 percent of people 65 years of age and older and 50 percent of people 18 to 64 years of age have one or more sites with
recession. The presence and extent of gingival recession also increased with age.
Results. More than 50 percent of the population has one or more sites with gingival
recession of 1 mm or more. The prevalence of gingival recession was found in patients with both good and poor oral hygiene. It has been proposed that recession is multifactorial, with one type being associated with
anatomical factors and another type with physiological or pathological factors. Recession has been found more frequently on buccal surfaces than on other aspects of the teeth.
Clinical Implications. Dentists should be knowledgeable about the etiology, prevalence and associating factors of gingival recession, as well as treatment options, so that appropriate treatment modalities can be offered to patients. Treatments for gingival recession include gingival grafting, guided tissue regeneration and orthodontic therapy. Such treatments typically result in esthetic improvement, elimination of sensitivity and a decreased risk of developing root caries.
Gingival recession is characterized by the displacement of the gingival margin apically from the cementoenamel junction, or CEJ, or from the former location of the CEJ in which restorations have distorted the location or appearance of the CEJ. Gingival recession can be localized or generalized and be associated with one or more surfaces.(Smith RG. 1997) The resulting root exposure is not esthetically
pleasing and may lead to sensitivity and root caries. As a result, we reviewed studies that described the prevalence, etiology and factors associated with gingival recession.
AGING
Similarly, Gorman found that the frequency of gingival recessio increased with age and was greater
in men than in women of the same age. Malpositioned teeth and toothbrush trauma were found to be the
most frequent etiologic factors associated with gingival recession.
Recession associated with labially positioned teeth occurred in 40 percent of patients 16 to 25 years of age
and increased to 80 percent of patients in the 36 to 86 years of age group. Those findings were corroborated
by Murray, who examined 4,000 subjects and found that the incidence of gingival recession increased with age.
ANATOMICAL FACTORS
One etiologic factor that may be associated with gingival recession is a prior lack of alveolar bone
at the site. The deficiencies in alveolar bone may be developmental (anatomical) or acquired (physiological
or pathological).Anatomical factors that have been related to recession include fenestration and dehiscence of
the alveolar bone, abnormal tooth position in the arch, aberrant path of eruption of the tooth and
individual tooth shape. All those anatomical factors are interrelated and may result in an alveolar
osseous plate that is thinner than normal and that may be more susceptible to resorption.
PHYSIOLOGICAL FACTORS
Physiological factors may include the orthodontic movement of teeth
to positions outside the labial or lingual alveolar plate, leading to dehiscence formation.Such
studies suggested that the acquired loss of alveolar bone might be associated with a number of identifiable
physiological or pathological conditions for which bone loss is part of a physiological or pathological
process.
PATHOLOGICAL FACTORS
Pathological factors include bone resorption as a sequel to microbially induced periodontal diseases.
In this case, however, the process of recession may be more complex since the teeth
involved may extrude, tilt and become mobile. A rat study demonstrated a possible mechanism of
gingival recession, showing that loss of attachment was the result of localized inflammatory
processes in connective tissue with the accumulation of mononuclear cells.(Baker DL 1976) It also was suggested that inflammation may persist subclinically and therefore cannot be eliminated as a factor in
recession.Similarly, recession has been related to inflammation in periodontal connective tissue
in monkeys.(Hopps 1974)
TRAUMA
In addition to psychological factors, various forms of trauma—such as vigorous toothbrushing, aberrant
frenal attachment, occlusal injury, operative procedures and tobacco chewing—have been thought to play a role in the etiology of recession.
Traumatic mechanical toothbrushing is factor in the etiology of gingival recession. The effects of toothbrushing have been studied by many investigators with general agreement that vigorous or incorrect use of the toothbrush can produce recession.
HYGIENE
The frequency of gingival recession in subjects with excellent oral hygiene has been reported to
be more frequent at buccal than proximal or lingual surfaces. In an epidemiologic study, gingival
recession was positively correlated with the frequency of toothbrushing.
Recession occurs more frequently in patients with good rather than poor oral hygiene.(O’Leary TJ 1971)
ABERRANT FRENAL ATTACHMENT
Aberrant frenal attachment also has been mentioned as a cause of localized
recession, but the evidence is not overwhelming. Some studies did not find any correlation
between frenal pull and recession, whereas thers did find an association.
CLASSIFICATION SYSTEMS
The Miller classification system.
A. Class I recession. B. Class II recession. C. Class III recession. D. Class IV recession.
TREATMENT OPTIONS
Different gingival grafting techniques have been proposed to treat gingival recession, including the lateral sliding flaps, coronally positioned flaps and connective tissue grafts, resulting in mean
root coverage of 65 to 98 percent. Guided tissue regeneration was introduced later to treat
recession, using bioabsorbable or nonabsorbable membranes, and studies showed similar results
with a mean root coverage of 48 to 92 percent. Orthodontic treatment can be considered with or
without periodontal surgery, especially in situations were teeth are malpositioned.
The etiology and prevalence of gingival recession
MOAWIA M. KASSAB, D.D.S., M.S.; ROBERT E.COHEN, D.D.S., Ph.D.
J Am Dent Assoc 2003;134;220-225
About different treatment techniques of gingival recession we will talk at future posts.
Subscribe to:
Comments (Atom)
Pages
About This Blog
Dental researches, publications, articles about Implant dentistry, aesthetic dentistry and Periodontology.
Blog Archive
-
▼
2010
(11)
-
▼
April
(8)
- Dimensional changes of the alveolar ridge contour ...
- Ridge preservation techniques for implant therapy ...
- Socket Augmentation: Rationale and Technique (Part 3)
- Socket Augmentation: Rationale and Technique (Part 2)
- Socket Augmentation: Rationale and Technique
- Socket Preservation technique before implant place...
- Subpontic osseous hyperplasia
- The etiology and prevalence of gingival recession
-
▼
April
(8)
Labels
- absorbable collagen dressing (2)
- collaplug (2)
- extraction sites (5)
- fresh extraction sockets (3)
- gingival recession (1)
- guided bone augmentation (4)
- human mineralized bone (2)
- human mineralized cancellous bone (2)
- immediate implant placement (2)
- immediate implants (2)
- implant placement (1)
- Puros (3)
- ridge presentation (2)
- ridge preservation (5)
- socket augmentation (6)
- Socket Preservation (6)
- Subpontic osseous hyperplasia (1)
- Zimmer Dental (2)
Followers
About Me
- Andrey Turkiv
- r3yand@mail.ru icq 7316646